Provider News and Updates
In the rapidly transforming world of health care, we understand how important it is for you to stay up to date on changes that affect you, your practice, and your patients. Below are notices, recommendations, and updates that can help you keep track of changing standards and regulations. Check back regularly for new postings.
Newsletters and Bulletins

Read the latest issue— Fall 2024
See the most recent Provider News updates.
Provider News
October 2024
August 2024
May 2024
February 2024
Bulletins
- Real-Time Prescription Benefits from Our Partner, MedImpact (July 18, 2024)
Provider News
October 2023
July 2023
February 2023
Bulletins
- SelectHealth Dental Survey (November 16, 2023)
- Medicare Webinar: Risk Adjustment & Quality Updates (October 5, 2023)
- Health Plan Provider Updates (September 7, 2023)
- Register now for our health plan portal (August 1, 2023)
- Medicare Webinar: Risk Adjustment & Quality Updates (July 14, 2023)
- NYRx Transition Period Ending 6/30/23 (June 22, 2023)
- Cabenuva, Apretude and Sunleca Coverage Information (May 11, 2023)
- Helping Patients with Daily Statins (May 9, 2023)
Provider News
November 2022
August 2022
May 2022
February 2022
Bulletins
- Members Getting New Plan ID Cards for 2023
- Mandatory Cultural Competency Training for SelectHealth Providers (November 8, 2022)
- SelectHealth Supports PrEP Aware Week 2022 (October 20, 2022)
- Closing Care Gaps in Vision, Dental, and Behavioral Health (October 13, 2022)
- VNSNY CHOICE Is Now VNS Health Health Plans (October 3, 2022)
- We’re Changing Our Name (September 29, 2022)
- Protecting Patients Living with HIV from COVID-19 (August 23, 2022)
- SelectHealth Members Get New ID Cards (August 16, 2022)
- Medicare Webinar: Documentation and Coding for Risk Assessment and Quality (June 30, 2022)
- Independent Assessor Process Started May 16 (May 23, 2022)
- Important News from VNSNY CHOICE (May 18, 2022)
- Medicare Webinar: Minding the Gaps (April 12, 2022)
- CAHPS Survey and HEDIS Audit for Total PCPs (March 8 ,2022)
- Some Capitation Payments Are Delayed to March (February 16, 2022)
Provider News
October 2021 (Two New Medicare Plans Join CHOICE Family)
Bulletins
- Closing the Asthma Medication Ratio Gap (October 19, 2021)
- Your VNSNY CHOICE Total Patients May Be Surveyed About Care You Provide
(March 2, 2021) - Alert Your Vendors: New Partner Handling CHOICE Online Transactions (February 25, 2021)
- Diagnosing and Treating Opioid Use Disorder (OUD) During COVID-19 (January 5, 2021)
Provider News
Bulletins
- Appeal a Claim or Dispute a Claim? (December 8, 2020)
- Provider Disclosure Certification Form Required by End of Year (December 1, 2020)
- Reassure SelectHealth Patients Needing Screens and Tests This Fall About the Safety of In-Office Visits (October 1, 2020)
- Real-Time Prescription Benefits from CHOICE Partner MedImpact Going Live October 1 (September 28, 2020)
- CHOICE Total Provider Update: Using Telehealth for HEDIS Measures (September 22, 2020)
- An Important Change for Arranging Non-Emergency Medical Transportation for VNSNY CHOICE Members (August 18, 2020)
- SelectHealth Celebrates SCOTUS Ruling on LGBTQ Rights (June 16, 2020)
- Use of Telehealth Services During the COVID-19 Public Health Emergency for CHOICE Total Medicare Providers (May 14, 2020)
- Use of Telehealth During the COVID-19 State of Emergency (March 27, 2020)
- Emergency Pharmacy Guidance for Prescribers (March 20, 2020)
- Helping Your CHOICE Total Clients with Surveys This Spring: LHCSAs and for PCPs (March 17, 2020)
- Appeal a Claim vs. Dispute a Claim (March 13, 2020)
- Novel Coronavirus and People with HIV: A Joint Statement from the NYC Health Department and the NYS Department of Health (March 13, 2020)
- Preparedness for COVID-19 (March 10, 2020)
- Opioid Safety Edits Were Implemented January 1, 2019 (January 7, 2020)
Provider News
Bulletins
- 2019 Provider Certifications (November 7, 2019)
- SelectHealth Expands to Westchester and Nassau Counties (October 27, 2019)
- Important Changes to Opioid Safety Edits for SelectHealth Providers (October 4, 2019)
New Member ID Cards for 2023
Effective January 1, 2023, members of the health plans from VNS Health have new member ID cards, reflecting the new names of their plans.
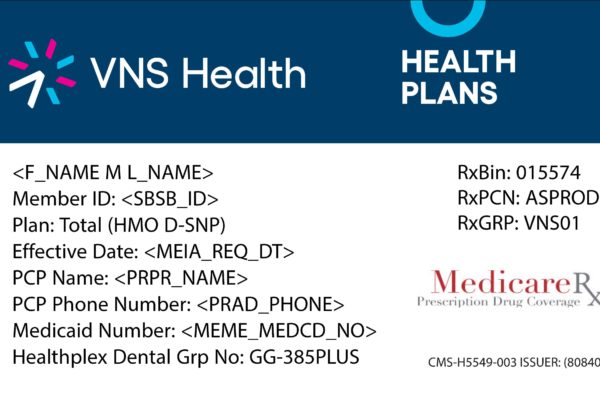
Medicare Plans
We have three Medicare plans: VNS Health Total (HMO D-SNP), VNS Health EasyCare (HMO), and VNS Health EasyCare Plus (HMO D-SNP). Our three Medicare plan cards look like this. You can find the plan name on the “Plan” line.
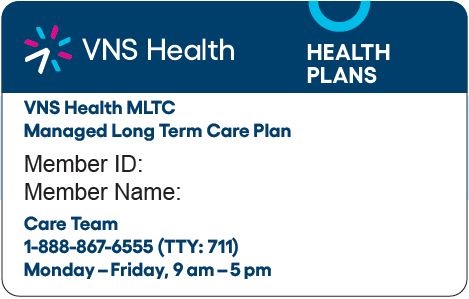
VNS Health MLTC
You may not see ID cards from our Managed Long Term Care plan, VNS Health MLTC, as they aren’t required to be shown for services. But in case you do, they’ll look like the card on the right after January 1.
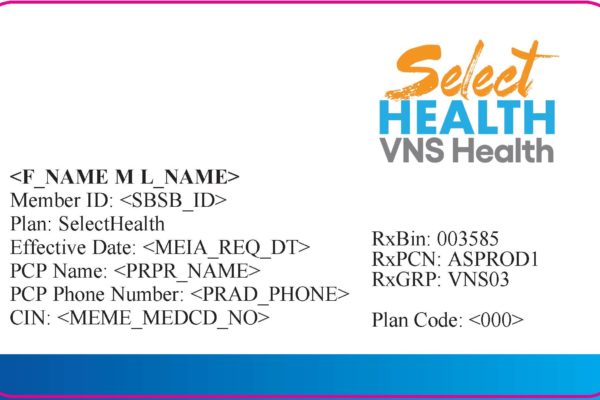
SelectHealth
We changed the name of our Medicaid special needs plan to SelectHealth from VNS Health and mailed out new ID cards last summer. SelectHealth member ID cards have a distinct look.
Guideline and Policy Updates
For All Health Plan Providers
This is a reminder that effective February 22, 2021, Availity is the preferred Electronic Data Interchange and portal vendor for VNSNY CHOICE Health Plans transactions.
You can also expedite your payments with electronic funds transfer. To receive electronic remittance advice files, enroll with Availity directly.
Please download this Provider News Update for more details.
Resumption of Prior Authorization Activities 7/7/2020:
Given the importance of medical review activities to CMS’ program integrity efforts, CMS will discontinue exercising enforcement discretion for the Prior Authorization Process for Certain Durable Medical Equipment, Prosthetics, Orthotics, and Supplies (DMEPOS) items beginning on August 3, 2020, regardless of the status of the public health emergency. For power mobility devices and pressure reducing support surfaces that require prior authorization as a condition of payment, claims with an initial date of service on or after August 3, 2020, must be associated with an affirmative prior authorization decision to be eligible for payment.
Additionally, prior authorization will be required for certain lower limb prosthetics (L5856, L5857, L5858, L5973, L5980, and L5987) with dates of service on or after December 1, 2020.
Please see more information here (PDF). The Required Prior Authorization list can be found here (PDF).
For VNS Health Medicare Providers
Cabenuva is on the pharmacy formulary for our Medicare plans. If you would like to initiate a plan member on Cabenuva, please send a prescription to a specialty pharmacy.
As part of a continued effort to alert VNS Health Total (HMO D-SNP) PCPs of member health changes in real time, we are pleased to announce the 2021 rollout of a new report containing member inpatient admission or discharge information.
Member PCPs should expect to receive this alert via secure email or secure e-fax each time a member is admitted and discharged from an inpatient facility.
We request that providers review the information upon receipt and enter all pertinent information into the patient’s medical record. Within the alert providers will find the following:
- Member demographic information
- Admitting provider, diagnosis, and date
- Discharge diagnosis, date, and length of stay (if applicable)
Other transitions of care best practices include:
- Schedule follow-up visits within 14 days of discharge (in office, in home, or telehealth)
- Conduct a medication reconciliation during a visit within 14 days of discharge, educating the patient or primary caregiver on any changes
- Tip: Code medication reconciliation in your electronic medical record to close quality gaps electronically:
- TCM visit codes meet the Medication Reconciliation measure and close gaps
- CPT code 99496 or 99495 for visits within 7 or 14 days, respectively
- CPT II ® code 1111F meets the measure for visits between 1 and 30 days of discharge
- TCM visit codes meet the Medication Reconciliation measure and close gaps
- Review any potential requirements for tests and treatments, and follow up as needed
- Coordinate with the health plans care manager for assistance with referrals for in-network specialists and other services
- Tip: Code medication reconciliation in your electronic medical record to close quality gaps electronically:
These alerts are aimed at assisting providers in meeting the HEDIS® Transition of Care (TRC) measure, among others. Two TRC measure components include:
- Documentation in the medical record that inpatient admission notification was received on the day of admission or the two following days (3 days total).
- Documentation in the medical record that discharge information was received on the day of discharge or the two following days (3 days total).
Thank you for your dedication to our members and their health.
If you have any questions, or if you would like transitions of care workflow training for your office staff, please contact the Quality Management team at [email protected].
VNS Health Total (HMO D-SNP) is pleased to announce its designation as a CMS Innovation Center Model participant for the Hospice Benefit Program. Learn more on our Hospice Benefit FAQs page.
New Guidelines for Telehealth Interventions in Four HEDIS Quality Measures
(For VNS Health Total Providers Only)
For SelectHealth from VNS Health Providers
As a SelectHealth from VNS Health network provider, you may find yourself in a position to provide trauma-informed care to Medicaid Managed Care (MMC) enrolled children/youth in direct placement foster care and in the care of Voluntary Foster Care Agencies (VFCAs).
Please download this letter for network providers for more information about the provision and coordination of services, pharmacy benefits, and the Initial Medical Assessment, which is required within the first 30 days of the child or youth’s placement.
Beginning April 1, 2023, all Medicaid members enrolled in SelectHealth will receive their prescription drugs through NYRx, the Medicaid Pharmacy Program.
Information about the transition of the pharmacy benefit from SelectHealth to NYRx, the Medicaid Pharmacy Program can be found HERE.
General information about NYRx, the Medicaid Pharmacy Program can be found HERE along with information for Members and Providers.
Provided are general important Medicaid Phone numbers below:
eMedNY 1-800-343-9000 for claims billing and ePACES help
Mon – Fri 7 AM – 10 PM. Sat – Sun 8:30 AM – 5:30 PM
Magellan 1-877-309-9493 for prior authorizations. Open daily, 24 hours.
1-800-342-3005 for medical supplies and procedure code limits
1-866-211-1736, Option 1 for enteral nutrition prior authorization
As of April 1, 2023, patients enrolled in SelectHealth and other NY Managed Medicaid Plans began receiving their pharmacy benefits through NYRx, the Medicaid Pharmacy Program. To help avoid disruption, NYRx instituted a transition fill period until June 30, 2023, enabling patients to receive a one-time transition fill for a 30-day supply of a drug that would normally require prior authorization (PA).
Starting July 1, 2023, all claims will be subject to NYRx pharmacy program criteria listed on the NYRx preferred drug list (PDL). If you haven’t already, follow up to confirm transition to NYRx is complete for your patients.
Please review the Preferred Drug List (PDL). Preferred products generally do not require PA when prescribed according to FDA labelling. For any products with clinical criteria that require confirmed diagnosis of FDA-approved or compendia-supported indication, please ensure you enter the diagnosis on the patient’s medical claims.
Click here for more information.
- Initiating PA for medications and diabetic testing supplies:
- Call Magellan at (877) 309-9493 – open 24/7
- Fax the PA form to (800) 268-2990
- Initiating PA for Enteral Nutrition Supplements:
- Call NYRx at (866) 211-1736, option 1
- Durable Medical Equipment (DME), Prosthetics, Orthotics, and Supplies (DMEPOS) procedures and supplies:
- Call OHIP DME at (800) 342-3005 for questions regarding DME PA criteria including frequency/quantity/durations limits and billing information
- Reminder: The items subject to the benefit transition are listed in Sections 4.1, 4.2, and 4.3 of the DMEPOS – Procedure Codes and Coverage Guidelines document and may be dispensed and billed directly to Medicaid through NYRx or by a FFS DMEPOS provider using the professional claim type. Most items do not require additional authorization prior to dispensing and billing.
The items not subject to the benefit transition are listed in Sections 4.4, 4.5, 4.6, and 4.7 of the DMEPOS – Procedure Codes and Coverage Guidelines document, and should continue to be billed to SelectHealth from VNS Health.
Helpful Links
Beginning April 1, 2023, all Medicaid members enrolled in SelectHealth will receive their prescription drugs through NYRx, the Medicaid Pharmacy Program.
To initiate provider enrollment with the New York State Medicaid program, visit https://www.emedny.org/info/providerenrollment/.
- Prescriptions written by licensed prescribers not enrolled in the NYS Medicaid Program will be denied effective April 1, 2023.
- Providers may check their enrollment status by reviewing the Medicaid Pended Provider Listing found here: https://www.emedny.org/info/ProviderEnrollment/ManagedCareNetwork/index.asp
- Questions regarding the enrollment process, your enrollment status, or what you need to do to enroll, please contact [email protected] or call the eMedNY Call Center at 1-800-343-9000
- Enrollment policy questions should be directed to the Medicaid Pharmacy Policy Unit by telephone at (518) 486-3209 or by email at [email protected].
New SelectHealth ID cards were recently mailed to all members. They look virtually the same as the old ID cards. The only difference is that they bear the plan’s new name, SelectHealth from VNS Health. Learn more.
OnTrackNY is an innovative treatment program for adolescents and young adults who have had unusual thoughts and behaviors or who have started hearing or seeing things that others don’t. OnTrackNY helps people achieve their goals for school, work, and relationships. Programs are located throughout New York State.
Eligibility Criteria
The program is for adolescents and young adults between the ages of 16 and 30 who have recently begun experiencing psychotic symptoms, such as hallucinations, unusual thoughts or beliefs, or disorganized thinking for more than a week but less than 2 years.
Services Offered by OnTrackNY
OnTrackNY utilizes a “shared decision making” model and involves:
- Comprehensive treatment using evidence-based practices delivered by an integrated clinical team specializing in early psychosis
- Psychiatric treatment, employment and educational support, substance abuse treatment, family education and support, CBT-informed individual psychotherapy, and other services as needed
How to Make a Referral to OnTrackNY
Contact your nearest OnTrackNY program site.
For SelectHealth members, effective 4/1/23, drugs, Cabenuva, Apretude, and Sunlenca are available under NYRx (pharmacy benefit). Prescriptions for these drugs can be billed by pharmacies to NYRx directly.
- To refer to NYRx reimbursable drug list, please use this link: https://www.emedny.org/info/formfile.aspx
- To refer to NYRx Preferred Drug List, please use this link: https://newyork.fhsc.com/downloads/providers/NYRx_PDP_PDL.pdf
For any questions related to coverage, please contact Magellan (NYRx) directly by calling, 877-309-9493
Sarepta
New York State has executed a state-direct supplemental rebate agreement with Sarepta for drugs used to treat Duchenne muscular dystrophy. This agreement went into effect on April 1, 2022.
Check the prescriber billing codes in the Reference Guides and Fact Sheets section of our Provider Toolkit for details.
Practitioner Dispensing Policy Clarification of DOH Billing Guidance (Effective 10/4/2022)
Check the prescriber billing codes in the Reference Guides and Fact Sheets section of our Provider Toolkit for updated information.
For drugs provided as part of a medical visit or incidental to a medical visit, Providers may bill covered drugs via the applicable J-Code and will be reimbursed based on the applicable drug fee schedule. (Access our Provider Manual for general billing guidelines)
To obtain the drugs, Providers may choose to:
- buy-and-bill – providers are responsible for ordering and purchasing the drug through source of choice and billing SelectHealth from VNS Health for reimbursement
- obtain directly from a Specialty Pharmacy within our medical network via:
white bagging (provider obtains an infusion or specialty drug directly from a specialty pharmacy)
brown bagging (drugs designated for self-administration or practitioner administration are dispensed or shipped directly to a member by the pharmacy. This is only acceptable when the drug is intended, prescribed, or labeled for self-administration).
For any questions about SelectHealth from VNS Health medical coverage related to Physician Administered Drugs (PAD), please call 1-866-783-0222, Monday–Friday, 8 am–5 pm. For claims and payment information and resources, please visit: https://www.vnshealthplans.org/health-professionals/claims-billing-and-payments/
To find a pharmacy in our medical network, please click the following link: https://www.vnshealthplans.org/health-professionals/search-for-in-network-providers/ and choose “SelectHealth Provider & Pharmacy Search”. Listed below are a few specialty pharmacies within our medical network:
- OptionCare Trinity – (800) 961-9979
- Mannings Pharmacy – (212) 941-6480
Billing guidelines can be found at the below location:
https://health.ny.gov/health_care/medicaid/covid19/guidance/billing_guidance.htm
Providers can contact [email protected] with any additional questions.
Billing guidelines can be found at the below location:
https://www.health.ny.gov/health_care/medicaid/program/phar_immun_fact.htm
Providers can contact [email protected] with any additional questions.
Patients enrolled in SelectHealth may be eligible for coverage for Zynteglo through NYRx, the Medicaid Pharmacy Program when certain criteria are met. The SelectHealth health plan can assist providers and members in obtaining approval for the medication through a few simple steps.
Once the health plan receives a request for Zynteglo, our team will send the patient’s physician a New York State worksheet for completion. Once the plan receives the completed worksheet, the plan will review New York State Medicaid criteria for coverage. If the member is eligible for the medication, the plan will facilitate communication of the eligibility with the state. NYRx will then work with a specialty pharmacy to dispense the medication.
For more information regarding the Zynteglo worksheet and clinical criteria information, please visit the following link here.